DEAR REHAB PROFESSIONALS, ITS TIME WE GET OUR SHIT TOGETHER
Getting injured sucks.
And yet every year, thousands of individuals experience the physical and psychological pain that comes with an injury requiring qualified medical intervention. Robbed of their physical freedom, people invest their time, money, and emotional standing on professions that promises to solve their problems. Whether it is regaining strength and confidence after an acute injury or ceasing daily pain and dysfunction – people need their rehab professional to be there for them.

Many clinics, and their clinicians, promise to “bridge the gap”, an industry buzzword to describe getting a person back into an active lifestyle. And they advertise it too! There, on their expensive ads in magazines, newspapers, and online pages, were those classic images I had seen since my earliest days as a practicing Physical Therapist. There was the smiling patient lifting a 2-pound dumbbell or pulling a TheraBand around the arch of their foot, and the promise of a smiling, yet authoritative, clinician to “bridge the gap” and get people back to their high-performance lifestyle.
What a bunch of shit!
Just because you use a buzzword or call yourself a “Transitional Therapist” does not make it true. It is disappointing to think about the reality of this practice
Yet another clinician is underloading their patients, wasting their time, and perpetuating the idea that rehab professionals have no concern over the actual physical capacity of those who trust them. And still, thousands of personal trainers will refer out blindly to these individuals, simply trusting their credentials and marketing after their client failed certain screens and assessments during a training intake.
And another client becomes a patient caught on the hamster wheel of pain, rehab, and the recommendation to “rest” while they heal. Another person is robbed of a life full of strength and physical freedom because their practitioner did not seek to empower them with independence, find ways to keep them training, or build them back better than ever with loaded training, pillar bracing, and proper breathing mechanics.
To be clear, this article is not referencing post-operation procedures or athletes returning to play. There is a significant difference between an individual recovering from an ACL reconstruction, a Hip Replacement, or a Tommy John surgery and the typical patient at a rehabilitation clinic. Additional articles can be written, and referenced, for these more complex situations.
With experience in training, therapy, and an obsession with making people stronger, empowered, and pain-free – I am on a mission to change the status quo, starting with this article and addressing everything missing in far too many rehabilitation practices. These are the changes every clinician and coach needs to make going forward if they truly care about “bridging the gap”.
DO NOT LEAVE THE GYM….OR STOP TRAINING

Ask anyone I have worked on, trained, or taught – my answer to the question “How do I get back into the gym?” has never changed. The answer is do not stop going…ever.
Here in 2021, we have more people than ever who are suffering from chronic diseases and co-morbidities. Obesity, diabetes, hyper-tension, and high cholesterol are literally taking people’s lives and yet, people are being instructed by licensed medical professionals to rest until a pain, or acute injury, “has healed itself” or given a script to a therapist who sees thirty patients a day and does not have the capacity to do more than the minimum.
For my patients, this approach has never worked in the past, and it is why they still need me after years of chronic pain, a further loss of capacity, and the emotional depression that comes from being, and feeling, broken. Ironically, had they found me originally, I am certain I could have addressed their initial problems quickly and had them on their way.
Instead, they ceased training and activity and found themselves a detraining statistic. In fact, studies have suggested that 2 weeks of immobilization resulted in measurable changes in muscle strength that requires over 6 weeks of training to return to baseline measurements. This is even more notable for aging populations, which if we are being honest, is a large segment of a clinicians schedule.
Another study demonstrated that reducing totals steps per day from 10,000 to 1,500 impaired insulin sensitivity, lipid metabolism, and contributed additional fat storage in otherwise healthy individuals.
Of course, certain individual factors are always in play, such as training history and current health condition, but the research is clear. Inactivity is the fastest route to weakness, deconditioning and additional health issues. Consider this – a patient is seeing you for an injury to a single shoulder…would you tell them to stop doing all other activities in the gym?
Unfortunately, many clinicians would recommend the cessation of loaded training until the injury is treated and the patient cleared. At best, they would be told to focus on their cardiovascular system with some walking or jogging – completely ignoring their opportunity to train legs, pillar stability, and *gasp* their other shoulder!
The evidence in support of the contralateral strength training effect (training a non-injured side) is nothing short of amazing. The best evidence suggests that training a non-injured side can create a 50% increase in strength in the effected side relative to strength progression of the trained side. This is because of a central mechanism and the potential for “spillover” of the neural control systems of the involved side. A great example of this is a patient in stroke rehab utilizing mirror therapy (which activates mirror neurons). Mirror-based therapy promotes changes at the cortical level (the brain) and can even induce changes in adjacent brain areas where an activity is mapped, stored, and performed via mirror neurons.
Or as any parent can relate, mirror neurons are exactly why your children can imitate your immature mannerisms in public and embarrass you.
And still, typical rehab seems to focus exclusively on rehabbing and “clearing” the injured side instead of improving the entire system. Once again seeing a single problem instead of the entire human.
There is no reason why a patient or client cannot train a non-injured side with intention and effort. A single arm chest press, row, or pulldown can provide mirror benefit to the upper body while a single leg press, split squat, or step up could do the same for the lower body. Even if a person is in a “non-weight-bearing” phase of their program – machines can be used to train the capable parts of their body and generate a fitness and performance benefit. A skilled clinician or trainer knows how to construct a safe and effective program to train around an injury.
The perfect symmetry would be a clinician rehabbing the injured area while the client continues to work with the strength coach for the non-injured areas. Unfortunately this type of collaboration is the exception, not the rule. Which is why you must commit to mastering your craft and caring endlessly for those who have trusted you. While it may lead to more work in-session and a wider-scope of practice – it will be worth in the long term when your client achieves full clearance without ever compromising their health and fitness.
EMPOWER INDEPENDENCE

Part of bridging the gap is giving a client, or patient, their physical, mental, and emotional independence back. Unfortunately, most practitioners overlook this aspect of their profession. It could be that 104 sessions a year is good for business, or it could be that there are another twenty people left to treat that day. It could even be that the clinician lacks the ability to work outside of the scope of their schooling.
Regardless of the reason why a clinician isn’t considering the power of instilling independence, now is when the rehabilitation field must change course. There must be intention in empowering a patient to take ownership of their recovery process, their return to activity, and the possibility that they could become better than ever.
When done correctly, rehab professionals are like tour guides, or Sherpas, that lead their patients down the right path, provide in-the-moment troubleshooting, and remain mindful of pitfalls and possible mistakes. A clinician should be with those who’ve trusted them through the summit.
Instead, the industry predominantly utilizes passive programming to keep the machine churning. The patient remains dependent upon their therapist to make good things happen while tepidly following some lazily assembled “home” program that has been used for over a decade on hundreds of people nothing like them. And just like our last bullet point highlights – there is little to no mention of exercise and in-gym training methods.
A clinician must figure out how to keep their patients in the gym training to improve their function, fitness, and performance. They must educate and empower their patients to perform more complex movement patterns like the squat, hinge, lunge, push, pull or carry. They must coach the importance of bracing and progressively loading tissues to influence positive adaptations of the physical body as well as the mind.
Training is empowerment.
Training is the living, breathing manifestation of independence.
Training is necessary.
And a patient/client must walk this road on their own, with professional guidance and instruction, to fully rehab any injury. They must gain the independence early in the process because their clinician empowered them to train around their injury, to build refined neuromuscular patterns, to become strong, physiologically free, and mentally tough.
A good rehab professional knows there is more to their job than prescribing 3 sets of 10 into the oblivion. They know a patient needs strength, resiliency, and independence. Does this sound like you? If not, then it’s time to re-evaluate your practice and do what is right.
STOP TRYING TO RECREATE THE PAST
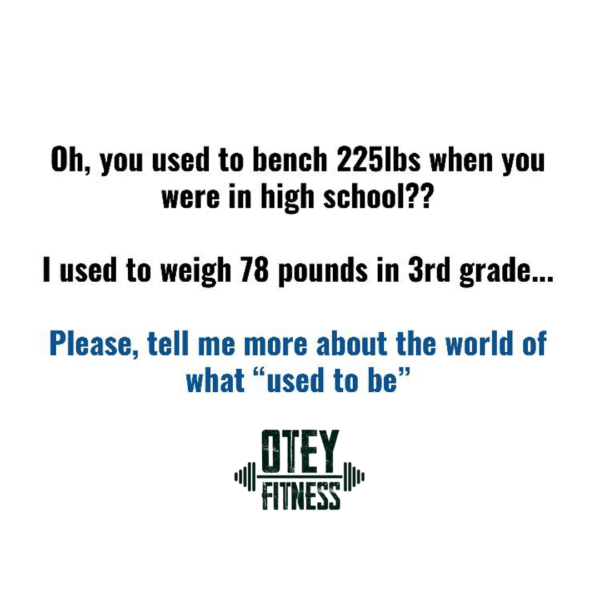
For years I thought nothing of a patient’s statement to “just get back to where I was before”. It seemed logical. Obviously, someone would like to be where they were before an injury. Yet, with time and more experience I couldn’t help but wonder why we were chasing the past when the future was sitting right in front of us. I mean really, why would any good clinician want to put you right back into the place, and the conditions, that led to your injury in the first place?
Instead, we need to build towards the future – just like any good counterparts in the fitness industry does with their training clients. Our goal as practitioners should be to make a patient better than ever when they leave our facilities, specifically when it comes to strength. We can, and should, make every patient we work with stronger. Strength is predictor of all-cause mortality, the foundation of physical and mental resiliency, and an achievement that no one has ever regretted. Really, has anyone ever said, “I wish I wasn’t strong”?
My job, our job, is to empower our patients with real training effects that positively impact their physiological, psychological, and emotional states and leverage the power of progressive overload and the SAID principle to make them better than ever.
STOP SEEKING THE UNICORN OF SYMMETRY

Humans are not symmetrical.
Yes, I just said that…and somewhere a functional guru spilled their matcha tea onto their BOSU ball in protest.
Seriously, we’ve become obsessed with this idea that a human should be perfectly balanced, especially when comparing range of motion within a limb (versus its opposite). I know hundreds of therapists and coaches who have done more harm than good with their obsession over a difference of 4.8575 degrees of motion between two joints.
I know them because at one point I was one. Regardless of who was in my office I was hell-bent on making sure that they left my care more symmetrical than a perfect square. Thankfully, I learned better in short order because my clients were not staying out of pain or were reinjuring themselves in training and life. My obsession with symmetry was a short-lived phase in my career but is the norm for many professionals practicing right now!
To be clear, this isn’t in reference to post-operation rehabilitation in which a surgically adapted joint should match a natural joint as closely as possible to ensure normalized functionality in life. This population does require more symmetrical measures in range of motion and strength (such as limb symmetry index or quad-to-hamstring ratios).
For the general population we are looking for “good enough”. Like a training screen, we are looking for proof that a patient can safely move and execute within an acceptable range of motion. As we coach in our PPSC material…ask yourself, “could I load this position?”
If the answer is yes, then move on and either address a connected region or prepare your patient to train. I liken this to how I fold clothes to avoid my wife’s disapproval – that look that every spouse who has thrown the clothes on the bed and called a day a time or two will know. As I fold, I ask myself…”is this good enough to avoid being yelled at?” If the answer is yes, then I move on. Sure, I might not be hired to fold for a major clothing brand anytime soon – but is that even my goal?
Sure, your client might not have perfectly symmetrical hips or shoulders, but is that even their goal?
With athletes, we must be extra careful with symmetry. It is quite possible that the sport the athlete participates in has influenced asymmetrical adaptations. Overhead athletes are the most prominent example of sport-specific adaptations, but even a sprinter like Usain Bolt provides context. His right leg is a half inch shorter than his left and yet he has sprinted past everyone numerous times and into the record books. At this point the weight of his gold medals probably cause more problems than his asymmetrical leg length. It is even possible, especially with throwing athletes, that the asymmetry is exactly why they have become a special performer. Maybe Usain’s legs gave him an advantage…or maybe they just didn’t impair him in a way that a clinician might think when only referencing the textbooks from our years of schooling.
Put simply, splitting hairs over a few degrees of extension or flexion is a misuse of time and the primary reason so many are stuck in rehab purgatory. Find good enough and begin empowering your patient with training effects that cause positive adaptation in the tissue. You can’t foam roll everything away.
MASTER BODYWEIGHT FIRST BUT PRIORITIZE LOADING
The saying, “learn to crawl before you walk” is a perfect euphemism for returning to training. Too often we see individuals add load to patterns which they don’t have neuromuscular control. As we would expect, more pain and injury occur.
It is important to own a pattern with no external forces prior to engaging in more advanced, or intense, training applications of a pattern. Everyone should be able to do a:
– Body weight squat before loading a squat.
– Body weight top down RDL before loading a hinge.
– A body weight lunge before loading a lunge pattern.
– Body weight push up before loading a push.
– Suspension trainer row (before considering a pull-up or cable-based pulling).
– Walk without extreme deviation before considering a loaded carry.

Individuals who cannot execute bodyweight loaded movements may need isolated attention on lagging muscles. Yes, it is true that muscles do not fire in isolation, as our functional guru brethren will scream from on top of their vibrating, ice-cooled, WiFi-Enabled foam roller. Yet, for many individual’s strength and efficiency of the motor units in a specific muscle tissue is the exact reason they can’t execute a pattern. So isolated training efforts on the lagging tissue might just unlock a pattern and higher-level functionality because in the end a stronger muscle in isolation is still a stronger muscle.
On the flip side of this coin, far too many rehab pros major in the minors. We obsess over optimal positioning (or symmetry) of a pattern and refuse to add significant load to it until an abstract metric is achieved. Instead of asking a client to achieve 50 perfect repetitions of a bodyweight squat in succession – why don’t you add 35-45% load to the pattern and allow type 2 fibers to join the party?
Loading is for more than just building muscles and enhancing performance – it is a critical element of a muscle’s function that when ignored in therapy could lead to another injury in the real world. Even if your client expresses zero desire to squat in a rack – it does not mean they won’t be lifting heavy objects during their next move or during a DIY project.
Load tissue with intelligence, with the intention of progressive overload and steady adaptation, but load it. Even light weight can be made to feel heavy if we coach the following two points appropriately.
GET TIGHT AND BUILD A BETTER PILLAR
Regardless of it you subscribe to the idea that injuries caused muscles to “deactivate” and become “out of sequence” on their firing patterns or not, one thing we can all agree on is that proper bracing and stabilizing techniques will help protect joints and non-contractile tissue. There are two huge principles that play into this.
The first is the concept of irradiation. Irradiation is a spread of muscle activation that augments postural stability and enables the transfer of power across joints by two-joint muscles.5. The best example of this is making a fist…

Squeeze your fist 25% of what your “peak” squeeze would be.
You probably feel some muscular tension in your hand and wrist, but not much else.
Now squeeze your hand at roughly 50% of your peak effort.
Do you feel the muscles of your forearms engaging?
Now squeeze 100% – like you are trying to punch a hole in a concrete wall
Wow. It spreads into the biceps, triceps, deltoid and your traps and lats.
This is irradiation and begin able to access it will literally make your joints more stable. It causes centration at ball-in-socket joints (more on that in a second) and enhances the neuromuscular function of the entire human movement system. It’s like a damn superpower when you use it correctly.
Ironically, most healthy people in the training population don’t understand how to leverage irradiation, so how do you think your patients who are injured and in painful, are doing? Adding this skill, this superpower, to their training program will rapidly accelerate their recovery process and provide a legitimate skill that carries over into life, training, and sport. Irradiation is like a complimentary ticket to strength, empowerment, and independence in training.
Once a person understands that they can get the muscles of their body to flex hard it is imperative to ensure that they can activate and utilize their pillar complex. The pillar is the active contraction of the functional stabilizers of the hips and shoulders (adductors, glutes, lats and pecs) coupled with the anterior core as a locking mechanism between the two. These actions build a powerful and effective brace for the body to load against. It protects the spine, the vital organs, centrates the ball-in-socket joints, and allows for the greatest possible expression of strength.
It is imperative to couple bracing with irradiation early in the rehab process (the first visit) as it will serve as the foundation for every single movement, exercise, and pattern in the clinic and in the gym.
When it comes to pillar function, we can use the developmental sequence (crawl before walking) to being to teach these principles.
Supine
Prone
Quadruped
Kneeling to half kneeing
Standing
We want to see the patient capable of executing the pillar brace and irradiation in these positions as well as within exercises and training modalities that are performed in these positions. But do not think you need to program overly complex tasks to create a lasting effect. Keep it simple and coach your patients/clients to brace what they want to protect.
Just Breathe…
The most common issue a patient will have once they’ve learned bracing mechanics is their pattern of breathing. They’ll most likely have little-to-no tension when they breathe normally and have little-to-no breathing when they reach sub-maximal tension (maximal tension typically involves the Valsalva maneuver). This final gap is one that when bridged – unlocks elite performance and a pain-free life. One could easily read and write a 5,000 word article on breathing alone, but I’d like to keep it simple.
Breathing and bracing go together like peanut butter and jelly. This relationship exists on a physical, mental, and even emotional level. Speaking purely anatomically – more attention must be paid to the diaphragm in core function discussions. Think of it this way:

If six pack abs are the front of the house, the diaphragm is the roof.
For someone to increase intra-abdominal pressure (brace what you want to protect), the lungs need to expand. This requires diaphragm to lower and the ribcage needs to be allowed to expand laterally. The problem that we see (especially in our chronic pain population) is that the use of compensatory breathing patterns, AKA “chesty breathing” that omit these functions. This impacts proper recovery and makes bracing nearly impossible to access.
Think about what happens when you hurt yourself.
The first thing you do is yell your favorite choice 4-letter word into the Universe. Then, your body reacts to the pain stimulus by pushing your body into a sympathetic state – the same state we’d use if we were running from an angry bear. This state does more than just make us more aware and increase our heart rate. It also increases respiration rate and activates secondary musculature (upper traps, scalenes, etc.) for breathing instead of leveraging the diaphragm and rib expansion. This shallow breathing might keep us alive in a moment of survival and allow for other functionalities to thrive, but it is a horrible way of living.
Living in a sympathetically charged state is a great way to wreak havoc on your endocrine, cardiovascular and neurological systems. A constant state of fight-or-flight caused by our work, commute, screen-time, intense workouts, and caffeine intake leave us stuck using our secondary respiration muscles for the predominance of our day. Now thrown pain in the mix and you have a non-stop cycle of redlining vital metrics.
I mean, since fitness trackers became a thing, we’ve all obsessed over how many steps we get in a day.
Why don’t we obsess over how many quality breaths we get in a day?
A normal respiration rate is 10-15 breaths/min. Expand this out over 24 hours and that gives an opportunity for 21,600 reps of breathing PER DAY. Dysfunction in the breathing pattern will negatively impact function up and down the kinetic chain. Pain-free living, peak functionality and a life of strength, empowerment and independence can’t be achieved if breathing is left dysfunctional.
We need to be teaching a 360-degree expansion (think of a cylinder) of the rib cage, the “diaphragmatic” breath, for our clients to thrive. This will not only allow them to brace and create appropriate tension but to also tap into the parasympathetic (rest and digest) system for recovery.
There are multiple different techniques on how to teach breathing. The developmental progression, as we highlighted in bracing above is the best approach due to gradual increase of gravitational and motor skill demands. Master 3D breathing in each position and your patient will access a new level of skill and capacity that they didn’t know was possible.
Breathing and pillar bracing are synergistic actions in the body and should be treated as such. These two actions are the foundation to any training pattern, loaded or unloaded, and a life lived pain-free. Mastering these concepts is far more important than that half degree of flexion difference between the right and left hip.
CONCLUSION
It’s time for the old way of rehabilitation to go out to pasture. It’s time for the winds of change to sweep through clinics across the country and provide a breathe of fresh air (under a Pillar brace) into a field caught up in its own insecurities and dogma.
Rehab should look like training.

Scratch that…rehab is training – with more controllable variables. It’s like bowling with the Bumpers up – you don’t need to use them, but they are there to protect against a major failure. Patients should be challenged by something more than 3 sets of 10 of the same TheraBand circuit that has been in circulation since Albert Einstein felt a pull in his groin.
The bullshit needs to stop and the life-changing effort to make light weight feel heavy so that heavy weight feels light needs to start. For me, it was my patient “Mo” that made this so clear.
“Mo” came to me after a diastasis recti repair due to 3 pregnancies within a very short period of time. She was left with absolutely ZERO core strength or stability, suffered from back pain, was unable to pick up her own kids without pain and almost falling over. All she wanted to do was return to a consistent gym routine which was unattainable for the past few years. Fast forward 3 months and “Mo” was repping out a new deadlift PR.
How did we get there?
We spent our initial 3 sessions teaching breathing, tension and bracing through developmental positions. I made sure she KNEW what pillar muscles felt like when working synergistically. We brought up all lagging areas with some isolated exercise focusing posterior and lateral hip, anterior core, low back, lats. And then we moved right into our 6 big foundational movement patterns- squat, hinge, push, pull, carry using patterns that she could own initially with body-weight and then progressively loaded over time.
Think about it; a PR in a deadlift during rehab…now that is bridging the fucking gap!




