THE CONCEPT OF “NO PAIN, NO GAIN” IS BULLSHIT

A sorry excuse of how to run a fitness facility because pain can be a potential warning sign of other serious medical issues. We need to move past the dogmatic “suck it up” mentality as this has only caused furthering a society that is broken down and hurt more than we are healthy. Yes, exercise is supposed to be hard and if you have lofty goals of getting that new squat PR then yeah, you are going to have to endure some pain. But that’s NOT the pain I am talking about. I am talking about the more serious symptoms (of which, pain is only a part) that can be potentially correlated to a much more serious underlying medical issue.
As a fitness professional, it is NOT in your scope to diagnose or even attempt to treat anything within the medical realm. However, fitness professionals have the most contact points with our clients. This is extremely important as it affords you an opportunity to let your client know they should be assessed by a clinician. Now, before we deep dive into identifying potential medical red flags let’s address the elephant in the room.
There is a distinct difference between muscle soreness and pain/clinical symptoms.
Some people (whether due to deconditioning or a lower tolerance to exercise) will have a hard time distinguishing between a muscle that is fatigued and sore due to exercise and something “painful” due to injury. Individuals can have a whole range of muscle soreness experiences from acute muscle soreness (begins immediately after a workout) to delayed-onset muscle soreness (DOMS) that begins 24-48 hours after a workout. While neither of these are medical emergencies, they are signs you may need to tweak some aspect of your program (volume, intensity, frequency, etc.) as soreness itself is not a good measure of a productive workout.
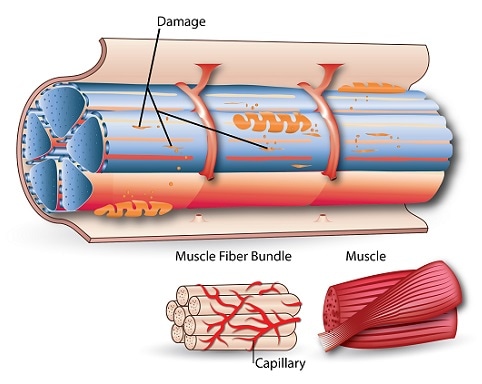
Diagram 1 – Delayed Onset Muscle Soreness (DOMS)
Again, the goal of this article is not to give freedom for a fitness professional to diagnose or treat any of these medical issues. It is also no to scare to shit out of you that everyone is going to have a medical emergency at the gym. Rather, it is to increase your awareness of instances where you should tell your client, “you should get that checked out” and to understand that it only takes one bad situation to potentially ruin your career.
Improve Your Intake Process
FIRST THINGS FIRST, YOU NEED TO HAVE A THOROUGH INTAKE PROCESS.

If you do not, you are doing a huge disservice to your clients. It amazes me when I have a room full of fitness professionals and ask how many have an intake process. Usually LESS THAN HALF the room raises their hands. This is a huge issue in the industry. If you do not have an idea of medical comorbidities than you are leaving your client at risk of injury or further medical problems. Yes, exercise is a great tool for health and wellness but if your client had a spinal fusion 5 months ago, cannot feel their foot because of surgery and oh by the way, is also is a type 2 diabetic who forgot to eat and check their blood sugar this morning then YOU are going to be the one held liable when they have a hypoglycemic episode during your back squat AMRAP and HIIT workout circuit. Getting to know people is one of the basics of being in any service industry. Take the time to get to truly know your people, this will only serve to drive success and safety as they train.
What is a Red Flag?
There are many different types of “flags” that we use in medicine to make a determination, should we move forward with treatment for this person or do we need to slam on the breaks. A RED FLAG refers literally to a sign/symptom that could be correlated to a serious pathology and generally requires further medical workup and testing. We are not talking about a sprained ankle. We are talking about things that could result in death or serious medical complications. Red flag literally means- stop and call 9-1-1. Don’t take 5 min, rub it and hope it gets better. Act immediately to take care of your client.
There are other flags that we can take into account. Yellow flags (for example) refer to how an individual experiences and holds beliefs about pain, emotional responses as well as pain coping strategies. This does not mean “don’t train and refer out” but it should be something you stick in the back of your head and be aware of. For example, a yellow flag could look like someone who believes that any type of soreness or fatigue means that there is some underlying structure that is “broken.” We know this is not true in most instances however, this can be a barrier and an area you as the coach may need to work around through education.
If you are a Personal Trainer/Fitness Professional who is unwilling to take these necessary steps for the health and well-being of your clients – let me introduce you to the White Flag. It’s time to surrender as an advocate for health and wellness as clearly it isn’t much of a priority for you.
Now we are on the same page of what a red flag is, the importance of an intake process and pain vs soreness, let’s take a deeper dive into four big red flags issues that you need to be aware of.
Red Flag Conditions To Be Aware Of
SPINE RELATED CONDITIONS
Spine-related pain and symptoms are some of the most common things that we see in the fitness industry. These can range from chronic low back pain to post-surgical clients. Serious etiologies of spine pain (including fractures, tumors, infections) are very rare and account for less than 1% of all medical cases seen for spine assessments.(1,2) In medicine, there are a lot of tests that are used to either rule in/rule out serious pathology. Diving into these examination techniques is not within the scope of this article. However, as a fitness professional, having a basic understanding of what needs referral is extremely important as your clients may be verbalizing serious issues just through conversation. Presence of serious pathology of the spine can be suggested by: (1) pain that is worse during rest vs activity, (2) pain that is worst at night, wakes individual up at night and is not relieved by any position.2 Other factors that require IMMEDIATE medical attention include:
- Blood in sputum (coughing up blood). This is NEVER normal, regardless of how hard the workout was.
- Any loss of conscious or altered mental status. This can be someone hitting their head or any change in mental status.
- Numbness or paresthesia in the perianal region. The region between your legs, never mess with ANY symptoms here.
- Pathological changes in bowel and bladder function. This can mean urinary retention or urinary incontinence. This is related to the above (#3) and a condition called cauda equina. There is a difference between drinking too much water and not being able to control your bladder.
Another serious sign to be wary of is any complaint of midline spine pain. This can be a little complicated due to all the muscles that attach onto the spine and it is possible for muscles to be sore due to a workout. I am referring to pain directly on the bone. This can be a sign of fracture (especially in your clients with osteopenia/osteoporosis), of spondylodiscitis (inflammation of the intervertebral disc), spondylolisthesis (fracture and slippage of the vertebra) or even other serious issues.2
When it comes to the spine (literally, the area where your spinal cord is located), do not mess around. If you see any of the above, make the appropriate call and ensure your client seeks out medical attention ASAP.
RHABDOMYOLYSIS

Diagram 2 – Rhabdomyolysis
I enjoy a brutal workout just like anyone else. I used to think if I wasn’t on the floor ready to pass out and seeing stars, then the workout wasn’t hard enough. I know there are many people out there who think this same way and who push themselves to their absolute limits. To make progress over time, this is important. However, pedal to the metal and straight up mindlessly programmed workouts with endless burpees, countless miles of running and AMRAP man-makers is just stupid.
Let’s be honest, any trainer in the world can make a workout hard but it takes mental effort and understanding exercise applications to make a workout effective.
Here is the reason this matters- exercise causes muscle breakdown. This is a normal occurrence. However, intense exercise past an individual’s tolerance level can result in disintegration of skeletal muscle which in turn causes leaking of muscle cell elements of myoglobin and creatine kinase (CPK) into the bloodstream and urine.(3) This is known as exercise-induced rhabdomyolysis (EIR). EIR can have serious complications including acute kidney failure, hepatic dysfunction, compartment syndrome, heart failure and in very severe cases, even death.3. At the anatomical level, EIR occurs due to myoglobin blocking kidney tubules (if present in large amounts for excretion) or myoglobin can be broken down by the kidney which produces highly toxic byproducts. These byproducts cause direct kidney damage.(4). If muscle damage is extreme the affected muscle tissue can swell drastically, become trapped within the borders of the surrounding fascia and result in muscle death.(4). This is known as compartment syndrome. Compartment syndrome usually requires medical intervention to avoid prolonged compression and ultimately, muscle death.
In terms of application, early warning signs of EIR include muscle swelling and prolonged/extreme muscle soreness beyond what would be expected based on duration and intensity. The fastest way to identify EIR is a urinalysis. Due to excessive myoglobin being leaked into the bloodstream, the individual’s urine will tend to be scarce, appear dark brown (this is usually referred to as “Coca-Cola” urine) and have a very strong smell.(5) The definitive diagnosis of EIR requires a blood test with CPK levels in excess of 10,000 U/L.6
Cases of EIR tend to occur more frequently after intense workouts that take place after an extended layoff (almost everyone getting back into the gym post-COVID), workouts that are novel/new, or a combination of both.(4) Heavy eccentric exercise has also had a higher correlation with EIR.4. A high intensity workout that can be tolerated by a very fit individual may be too much and a cause of EIR for someone who is deconditioned.
This has a large application to and fitness facility but especially group fitness settings due to it being harder to control every aspect of a class. Again, this should drive home the point that you need to have some sort of intake process and you NEED to know your people. If you have no idea of an individual’s conditioning level then you could very literally be sending them to the ER. When in doubt, defer to more frequent concentric and isometric exercise selections and allow acclimation periods so you don’t become that coach that does “too much, too soon, too fast”.(7)
DIABETES AND HYPOGLYCEMIA
We have all made this mistake. You wake up late and forget to eat breakfast before your workout. Midway through, you are getting clammy, shaky and feel like you are going to pass out. Literally, you are the embodiment of every Snickers commercial ever created. For a lot of people, this experience (although unpleasant) is not a deadly. If your client is a diabetic however, this situation can quickly become a medical emergency.

The literature is well versed in the important of exercise in health management for those individuals with Type 1 (T1DM) or Type 2 (T2DM) diabetes which means we will all work individuals who have this co-morbidity.(8) Specifically, exercise in this population helps with weight loss management, peripheral insulin sensitivity, glucose uptake and utilization as well as cardiovascular health.(8) However, the largest reason that this population DOES NOT exercise is actually due to fear of a hypoglycemia episode.(8) So we have a population who is fearful to utilize the very thing that can improve their health in the short and long term. This is why fitness professionals need to have a basic understanding of how to identify a hypoglycemic episode.
To review, our bodies release insulin in response to eating carbohydrates. Insulin is a hormone whose main job is to drive glucose into cells for storage or utilization. This process allows blood sugar levels to return to normal after a meal. There is also a secondary system that allows muscles to uptake and use glucose independent of insulin. Simply stated, individuals who have diabetes are unable to regulate blood glucose which can result in excessive blood glucose (hyperglycemia) and in severe cases with insulin overdose, low blood glucose (hypoglycemia) as well.
Due to the importance of and emphasis placed in managing blood glucose, there can be negative consequence of a hypoglycemic episode during exercise. These occur more often in individuals treated with insulin. What typically occurs is that insulin requirements exceed metabolic requirements and when compounded with blunted neuroendocrine, autonomic nervous system and metabolic counter-regulatory responses, hypoglycemia-associated autonomic failure can occur.(8) In simpler terms, your client can end up with diabetic shock (severe hypoglycemia) which can result in seizures, coma and even death. In even less severe cases of hypoglycemia, cardiovascular integrity may even be affected.(8) It is also important to note that hypoglycemia can occur immediately after and even up to several hours after exercise. This is why it is important to educate our clients in this population about the importance of adequate carbohydrate consumption during and after exercise.
The American Diabetes Association has concluded that exercise guidelines developed for nonspecific populations can be applied to individuals with T1DM or T2DM and recommendations from the ACSM suggest that individuals with diabetes be medically screened for diabetic complications prior to beginning an exercise program.(8) There are also guidelines for exercise in T1DM and T2DM to help avoid an emergency. These include monitoring blood glucose before and during exercise as well as immediately after and several hours after exercise specifically for those individuals who take insulin. Once typical glycemic responses are determined based on activity, continued glucose monitoring is important especially if the individuals is changing diets, bodyweight or exercise intensity/duration.8. Other recommendations from the ADA including supplementing with carbohydrates if blood glucose is below 100 mg/dl prior to the start of exercise and avoiding exercise for 24hours after a hyperglycemic episode.
ADA guidelines also suggest consuming 10-15 g of carbohydrate to prevent exercise-induced hypoglycemia however further research has suggested that carb intake needs to individualized to the type of insulin and absorptive state.(8) Typically, an individual who is experiencing hypoglycemia may report headache, dizziness, sweating, shaking and a feeling of anxiety. Early recognition and treatment of this is essential because if blood sugars stay low for too long, a diabetic coma could be the result. Your best go to carbohydrate drinks include- orange juice, skimmed milk, whole milk, a sports drink with carbohydrates and electrolytes.(8) All gyms, clinics and fitness facilities who knowingly work with this population should have these drinks on hand in case of a medical emergency. If you encounter someone who fits the mold of a diabetic hypoglycemic event, do not hesitate to act. By the time 911 arrives, it could be too late.
CHEST PAIN

Heart disease is the LEADING cause of death for men and women in the United States. Heart disease is so prevalent that one person dies every 36 seconds due to CV disease.(9) As with diabetes, this is a population who NEEDS physical activity to not only improve their health but to also stay alive. There is a HUGE difference between someone being out of breath and someone experiencing a cardiovascular episode. The reason individuals get chest pain during exercise is due to increase oxygen demand from the heart. In a normal, healthy heart, the heart will beat faster to increase blood flow (oxygen) to the rest of the body. In a heart that is diseased and has any sort of blockage, this increase demand cannot be met due to blood vessels not being able to dilate. This can ultimately cause a heart attack (an oxygen problem) and potentially, cardiac arrest (an electrical problem) with the latter requiring immediate AED use. Some symptoms of cardiovascular disease during exercise include: pressure, tightness, squeezing sensation in the neck and down the left arm, nausea, shortness of breath, hot and cold sweats.
Women generally demonstrate uncommon symptoms of CV disease even though men are more likely to have it.(9) One of the hardest aspects about cardiovascular disease is that more times than not, there are no symptoms. This is why the fitness professional needs to be able to recognize and respond quickly in any cardiovascular event. If, at any point, your client starts complaining of chest pain, you should discontinue all exercise and get that individuals to their physician. Again, there is a big difference between out of breath because I am out of shape and someone out of breath, dizzy, nauseous and complaining of chest pain. Know the difference and act quickly.
Conclusion
If exercise were a pill, it would be the most prescribed pill in the history of mankind. Exercise is proven to help slow down and even in some cases completely reverse significant disease. This is why it is important to have a basic understanding of medical red flags because the people who need exercise the most are the people who have the most comorbidities and who are the most likely to exhibit a medical red flag. Although it is out of your scope as a fitness professional to medically diagnose or offer medical advice to anyone who steps foot into your facility you must be aware of the situations that can result in your client becoming permanently disabled or even losing their life. These instances are extremely rare in fitness however it only takes that one act of negligence to alter someone else’s, and your, life trajectory forever.
References
-
Wilk V. Acute low back pain: assessment and man- agement. Aust Fam Physician. 2004;33:403–407.
-
Sizer, PS, et al. Medical Screening for Red Flags in the Diagnosis and Management of Musculoskeletal Spine Pain 2007, Pain Practice. Volume 7, Issue 1, 2007 53-71.
-
Sunder A, Mohanty B, Singh A, Yadav P. Rhabdomyolysis – Exercise induced nightmare. J Family Med Prim Care. 2019;8(1):305-307. doi:10.4103/jfmpc.jfmpc_370_18
-
Rider, BC., Exertional (Exercise-Induced) Rhabdomyolysis. ACSM Health and Fitness Journal, May/June 2019.
-
KahnF. Rhabdomyolysis: a review of the literature NethJMed.2009;67:272–83.
-
KimJ,LeeJ,KimS,RyuYoungH,ChaSK,SungDJ.Exercise-inducedrhabdomyolysis mechanisms and prevention: a literature review. J Sport Health Sci. 2016;5:324–33.
-
Eichner ER. Football team rhabdomyolysis: the pain beats the gain and the coach is to blame. Curr Sports Med Rep. 2018;17:142–3.
-
Younk LM, Mikeladze M, Tate D, Davis SN. Exercise-related hypoglycemia in diabetes mellitus. Expert Rev Endocrinol Metab. 2011;6(1):93-108. doi:10.1586/eem.10.78
-
Heart Disease Facts. https://www.cdc.gov/heartdisease/facts.htm
-
https://www.heart.org/en/health-topics/heart-attack/about-heart-attacks




